Testosterone
| Testosterone | |
|---|---|
| |
| General | |
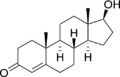
| Systematic name | 17β-hydroxy-4-androsten-3-one |
| Molecular formula | C19H28O2 |
| SMILES | CCCCCCC(=O)OC1CCC2C1 (CCC3C2CCC4=CC(=O) CCC34C)C |
| Molar mass | Molar mass::288.4g/mol |
| Appearance | White/creamy white, in the form of solid crystals |
| CAS number | CAS number::58-22-0 |
Testosterone is the major sex hormone in males. It does many things to males during their period of puberty, and even further on. It gives them muscles, deepens their voice, increases the size of their adam's apple, and can sometimes be the cause of aggressive actions as they try to sort out their feelings as they grow into men. While testosterone may turn boys into men by giving them muscles or facial hair, it is also the hormone that is responsible for the production of sperm, giving males the ability to have children when they are finally settled with their wives. God manufactured the very first testosterone molecule with the very intent that it would give humans the joy of having children and watching them grow up into the people that they were meant to become. As God created man on the sixth day of creation, he gave men testosterone and women estrogen in order that they may have the joy of having someone to call their own.
Structure
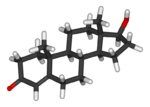
Testosterone is a steroid hormone, and, like most other steroid hormones, is derived from cholesterol, which is a sterol lipid with the chemical formula C27H45OH. [1] [2] Steroid hormones are characterized by a carbon skeleton with four fused rings that are part of their molecular structure. They are distinguished by the functional groups attached to these four rings. A major class of steroid hormones that are responsible for the development of the male secondary sex characteristics are androgens. Testosterone is derived from the androgen called androstenedione via a reduction of its 17-keto group. [3]
The presence of a hydroxyl group (-OH) at position C-17 has enabled the development of synthetic forms of testosterone that can be administered in therapeutic treatments:
- Through the esterification of testosterone, which is the substitution of an acid group for the hydroxyl group, the water solubility of the molecule is lowered and its lipid solubility is increased, which permits a sterile oil-based injectable to form a “depot” in the muscle, from which it is gradually released.
- The hydroxyl side chain at the C-17 position also permits the alkylation of the steroid molecule, which is the substitution of an ethyl or methyl group for the hydroxyl group. Alkylation enables the development of oral steroids, which can be taken up by the digestive track, and can then be easily administered to the patient in pill form. [4]
Production
Most hormones in the body are synthesized in a specialized tissue, and are then released to their target cells as needed. In men, the largest amount of testosterone is produced by the testes. However, it is also synthesized in smaller quantities in women by the thecal cells of the placenta, the ovaries, and the zona reticularis of the adrenal cortex in both genders. Testosterone is specifically produced by Leydig cells in the testes of males. The male generative glands also contain Sertoli cells, which require testosterone for spermatogenesis, which is the synthesis of spermatozoa. Testosterone is not soluble in water, so it is transported to target cells bound to a specific plasma protein called sex hormone binding globulin, abbreviated SHBG. When the hormone arrives at the target cell, it binds to a site on the receptor protein. This binding creates a ligand-receptor complex, which causes a conformational change, or a change in the molecule's structural arrangement, that initiates a sequence of reactions leading to a change in cellular function. [5]
A signal is sent from the brain to the pituitary gland at the base of the brain control the production of testosterone in men. The pituitary gland relays signals on to the testes to produce testosterone. A "feedback loop" is what regulates the amount of hormone in the blood very closely. When testosterone levels rise too high, the brain sends signals to the pituitary to reduce production.
Effects
Testosterone also tends to have many effects during puberty in males. The main things that the testosterone hormone can cause are:
- Phallic enlargement
- Increased libido and frequency of erection
- Pubic hair extends to thighs and up toward umbilicus
- Facial hair (sideburns, beard, mustache)
- Chest hair, periareolar hair, perianal hair
- Subcutaneous fat in face decreases
- Increased muscle strength and mass
- Deepening of the voice
- Growth of the adam's apple
- Growth of spermatogenic tissue in testes; male fertility
- Growth of jaw, brow, chin, nose, and remodeling of facial bone contours
- Shoulders widen and rib cage expands
- Completion of bone maturation and termination of growth. This process occurs indirectly via estradiol metabolites, and tapers off more gradually in men than in women.
Deficiencies
A deficiency with testosterone, often referred to as low testosterone, is called hypogonadism. [8] There are many different symptoms for testosterone deficiencies. These may include:
- a decreased sex drive
- a decreased sense of well-being
- a depressed mood
- some difficulties with concentration and memory
- an erectile dysfunction
There are also several changes in the body that may occur when the body has a testosterone deficiency, including:
- a decrease in muscle mass, with an increase in body fat
- variable effects on cholesterol metabolism
- a decrease in body hair
- fragile bones (osteoporosis)
- a decrease in hemoglobin and possibly mild anemia
- a low sperm count
- enlarged breasts
One of the ways that a man can have a testosterone deficiency is simply through the process of time. As a man ages, the amount of testosterone in his body will gradually decline, usually starting after a man is thirty years old. This steady decline will then continue throughout the rest of his life. While this decline is rather poorly understood and its significance is controversial, there are many other potential causes for testosterone deficiency. Some of these may include:
- an injury or infection to the testicles
- AIDS
- hemochromatosis (too much iron in the body)
- an inflammatory disease such as sarcoidosis (a condition that causes inflammation of the lungs and other organs)
- a genetic abnormality such as Klinefelter’s Syndrome (extra x chromosome)
- stress
- uses of medications, including hormone analogues used to treat prostate cancer and steroids
- alcoholism
- a session of chemotherapy or radiation treatment for cancer
- a chronic illness
- a cirrhosis of the liver
- dysfunction of the pituitary gland (a gland in the brain that produces many important hormones)
- a chronic renal (kidney) failure
- congenital conditions, Kallman’s Syndrome (low hormones, inability to smell and other abnormalities)
Tests
Testosterone Tests may be performed if the patient has symptoms of abnormal male hormone, or androgen, production. The testes produce most of the circulating testosterone in men, and the ovaries produce most of the testosterone in women. In males, a hormone known as LH from the pituitary gland is what stimulates the Leydig cells in the testicles to produce testosterone. In females, the adrenal cortex produces another male hormone, called DHEAS. [13]
There are many accurate ways to test yourself for your testosterone levels to prove whether or not you have a deficiency, but the best is to have your doctor measure the amount of testosterone in your blood. To test for a possible deficiency, it can take several different measurements of testosterone due to its fluctuating levels throughout the day. The highest levels of testosterone are usually in the morning, which is why doctors tend to conduct the tests in the early morning. [14] [15] Other possible ways to test for a deficiency would be to have the physician examine the amount of body hair on the patient, their breast size, the size and consistency of their testes, scrotum, penis size, and their ability to see in all directions. [16] Your doctor or physician may ask you to prepare for the test by asking you not to take drugs that may affect the test. [17]
When the test is performed, the physician will draw blood from a vein, usually from the inside of the elbow or the back of the hand. The site is first cleansed with a germ-killing medicine called antiseptic. Then the physician will wrap an elastic band around the upper arm in order to apply pressure to the area of the site where the blood is to be drawn from. This will make the vein swell with blood. Then the physician will gently insert a needle into the vein, collecting the blood into an airtight vial or tube attached to the needle. The needle is removed after the blood has been collected, and the punctured area is covered in order to stop the bleeding. [18]
There are some risks with the performing of the test. Veins and arteries do vary in size from one patient to another and from one side of the body to the other, causing the obtaining of a blood sample from some people more difficult than from others. Other risks that are associated with having blood drawn are rare, but may include:
- excessive bleeding
- fainting or feeling light-headed
- hematoma (blood accumulating under the skin)
- infection (which is a small risk any time the skin is broken)
The testosterone levels are used to assess for a deficiency, as well as:
- early or late puberty in boys
- possible impotence and infertility in men
- any excessive hair growth, male body characteristics (virilization), and irregular menstrual periods in women
The normal results on such a test would be:
- 300 -1,000 ng/dl (in men)
- 20 - 80 ng/dl (in women)
(ng/dl = nanograms per deciliter)
There are sometimes abnormal results for the test. If a patient has an increased production of testosterone, he/she may be suffering from any of the following:
- androgen resistance
- congenital adrenal hyperplasia
- ovarian cancer
- polycystic ovary disease
- precocious puberty
- testicular cancer
If a patient has a decreased production of testosterone, he/she also may be suffering from any of the following:
- chronic illness
- delayed puberty
- hypopituitarism
- prolactinoma
- testicular failure
There are some considerations that must be taken into account before having the test done. More sensitive tests do measure the total amount of testosterone in the blood, but they can also determine how much of that total amount is "free" or "bioavailable" testosterone. [19]
Replacement therapy
The options for testosterone replacement therapy can sometimes vary, but there are usually only three. They are:
- intramuscular injections, usually taken every two or three weeks
- testosterone patches worn on either the body or the scrotum (the sac that contains the testicles). These patches are to be used daily for maximal results. The body patch application is rotated between the arms, the buttocks, and the back or abdomen
- testosterone gels that are applied daily to the shoulders, the upper arms, or the abdomen
- tablets (stick to the gums)
Each of these treatments is designed to provide adequate levels of hormone replacement. While most of the effects of the treatments are to the patient's advantage, there are some disadvantages, or side effects, as well. The intramuscular injections can produce wider swings in the concentration of the hormones, with higher levels shortly after the injection and lower levels just before the next injection is due. They may also produce increases in the blood cell count that are higher than normal. The body patches can produce skin irritations in a rather significant number of men, which causes the use of the patch to be discontinued. The testosterone gels require special care to make sure that the hormone is not accidentally transferred to another person or partner.
Other common side effects from testosterone replacement therapy may include:
- acne or oily skin
- breast enlargement
- decreased testicular size
- mild fluid retention
- stimulation of prostate tissue, with perhaps some increased urination symptoms such as decreased stream or frequency
- worsening of sleep apnea, which is a sleep disorder that results in frequent night time awakenings and daytime sleepiness
There are also some rare side effects that have been experienced in testosterone replacement therapy, such as:
- changes in cholesterol concentrations
- increase in red cell count
- decrease in sperm count, producing infertility (especially in younger men)
Currently, there are no pills in America available that can provide the adequate levels of hormone replacement in a male. In addition to this disadvantage, oral medications can produce liver abnormalities and should be avoided. The best choice of hormone replacement therapy is made with a thorough discussion between a patient and his physician. [26]
While testosterone replacement therapy can be a good thing, there are those who should not have it done. It can stimulate growth of the prostate, which can lead to prostrate cancer if it is already in the early stages of development. Thus, men with prostrate cancer should not have testosterone replacement therapy, because it will worsen their condition. A prostrate screening is recommended before having the procedure done. Along with prostrate cancer, those men with the rare condition of breast cancer should also avoid testosterone replacement therapy. [27]
In general, testosterone replacement therapy is a relatively safe procedure. If you are taking hormone replacement therapy, regular follow-up appointments with your physician are important. [28]
There have been interesting speculations of doctors about whether or not testosterone therapy can help increase sex drive in menopausal women, but there's no consensus among them about the benefits and risks of testosterone therapy for menopausal women. While testosterone is one of the hormones that contributes to a healthy sexual function in women and testosterone therapy could help, it typically, however, isn't recommended to improve low sex drive. For women, other factors are generally more important in determining sex drive than testosterone, and since much remains unknown about the effects of testosterone therapy in women, it is safer to leave it alone until doctors know more about the effects that it could have on the female anatomy.
Typically, testosterone therapy isn't recommended for women in general, especially those who are postmenopausal and can't, or choose not to, take estrogen. Testosterone therapy isn't appropriate for postmenopausal women who have a history of breast or uterine cancer or those who have cardiovascular or liver disease. For women, testosterone therapy may be given in the form of either a cream or gel, and sometimes it may be prescribed as a pill or injection. There have been not been any long-term studies of the risks and benefits of testosterone therapy in women, making it rather risky. The most common side effects of testosterone therapy in women include:
- acne
- excessive facial hair
Less common side effects include:
- lowering of the voice
- enlargement of the clitoris
- liver problems
- mood or personality changes
References
- Testosterone Replacement Therapy
- Testosterone
- What Causes Low Testosterone Levels?
- Does testosterone therapy help menopausal women?
- Testosterone — What It Does And Doesn't Do
- Testosterone
- Testosterone Enanthate
- Physical properties of Testosterone
External Links
- Definition of Testosterone
- Testosterone
- Transdermal Testosterone Treatments
- Calls for testosterone trials in CHD