Streptococcus pneumoniae
| Streptococcus pneumoniae |
|---|
|
|
| Binomial Name |
|
Streptococcus pneumoniae |
Streptococcus pneumoniae is a bacteria that can cause pneumonia, peritonitis, sinusitis, middle ear infections, otitis media, meningitis, arthritis, and bacteremia in most humans, mice, rabbits, monkeys, and horses. There are more than ninety different sterotypes of streptococcus pneumoniae, which makes it very hard to get rid of. It is usually harmless, but if the circumstances go bad, it will become a disease.
Anatomy
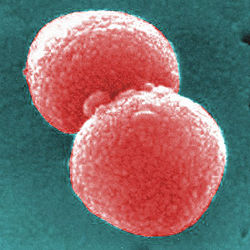
The cells of streptococcus pneumoniae are cocci (round bacterium) with a distinctive lancet-shaped. The diameter of a S. pneumoniae cell is usually somewhere between .5 and 1.25 micrometers long. When observed, they are usually viewed as a diplococci (occuring in pairs of two joined cells), but occasionally are seen singularly and in short little chains. They are Gram-positive, which means they keep the color violet when they are Gram stained. [1] Scientists have discovered the shape of the molecule that S. pneumoniae (unable to move by itself) uses to catch hold of the cells that line the lungs and the throat. The molecule is called CbpA, which is large and paddle-like. CbpA is a really important discovery, S. pneumoniae being the only bacteria that is known to get into cells by using CbpA to bind onto pIgR. Now that the shape of it is known, it will be easier to make a vaccine that can be more successful in kids. Streptococcus pneumoniae do not have catalase. Differently than other bacteria in the genus Streptococcus, S. pneumoniae don’t show an M protein, and their cell wall is very important. It is around six layers thick, and in experiments, when the cell wall components are confronted, disease symptoms are created. Lately, there have been reports of hair-like structures that extend from the surface of S. pneumoniae, and that apparently have contributed in colonizing. [2] [3]
Reproduction
Streptococcus pneumoniae grows best in five percent carbon dioxide. It always needs a catalase base to be able to grow on agar plates. When it is on agar plates, they grow in colonies with a diameters of about 1 mm. Two different types of S. pneumoniae develop; a transparent type and an opaque type. The opaque type survives in blood the finest, and the transparent type is the type that colonizes in the nasopharynx the best. The catalase neutralizes the hydrogen peroxide that they make. When grown in culture it needs the environment to be totally anaerobic about 20% of the time. It isn’t able to make a catalase by itself. When the setting is about ninety-eight degrees Fahrenheit, Streptococcus pneumoniae is able to double in around twenty minutes to a half an hour. They also contains an enzyme called an autolysin that is able to cause the host organism to kill itself. Whether there is an autolytic enzyme in it makes the difference of whether medicines can get rid of the organism’s cell wall. It shares that skill with two other bacterias that are normal invading bacteria. [4] [5]
There was a space shuttle that took streptococcus pneumoniae into space for eight years to see how it changes when it’s in microgravity and to discover if it is a potential harm for astronauts who will be in space for a while, who wouldn’t have a chance for a fast trip back to earth. People's immune systems function slower the longer they’re in Space; bacteria have been shown to grow faster in microgravity. The scientists who had arranged for it to be sent into space had started a project called "Streptococcus pneumoniae: Expression of Genes in Space," (SPEGIS) in 1999. Endeavour, the space shuttle it was sent on, came back to the Kennedy Space Center on August 22, 2007, and were in sealed experimental containers, frozen. [6]
Ecology
Even if the people are healthy, Streptococcus pneumoniae is present in the nasopharynx of about twenty to forty percent of children; but the reported numbers can vary to even up around fifty percent, and five to ten percent of adults who are healthy, or even as high as thirty percent for adults. However, there are a lot of aspects that would change the numbers of people with S. pneumoniae, like age, and depending on age, daycare or similar things (for example, if not attending daycare it would be less likely for a kid to have it, and even immunity and antibiotics that are used by the person would be a factor.) It is normally just colonized in the nasopharynx, but it turns into an infection if it is brought into an area where it is not eagerly accepted, like the Eustachian tube or nasal sinuses. That could happen if there were allergies or viral infections there.
When Streptococcus pneumoniae is breathed into the lungs and not destroyed, it becomes the cause of pneumonia. If the organism goes to a place where it isn’t usually, the complement protein group stimulates cytokine production, and white blood cells are attracted. The bacteria can’t be effectively destroyed by the polysaccharide capsule alveolar macrophages. Because of that, it is spread to the blood stream. It can cause otitis media and paranasal sinusitis, meningitis, brain abscess, or septic arthritis after being carried to the meninges, bones, joint spaces, and peritoneal cavity from the blood stream.
When someone is known to have S. pneumoniae, they are treated with antibiotics. Penicillin is one of the antibiotics that has worked effectively in treating it, but like other bacterium, S. pneumoniae has gotten more and more resistant against antibiotics used previously in other people. There is a vaccine that is recommended for all kids for S. pneumoniae, but if a kid gets a different sterotype of the bacteria that isn’t in the vaccine, the kid could still get sick from it. Colonization of S. pneumoniae has lessened because of kids getting vaccines, and in other members of their family because of herd immunity, where so much of the population is immune that the bacteria can’t get a new host. Smallpox was gotten rid of by herd immunity.[7][8] [9]
Diseases and Symptoms
One of the best known diseases that can be created when Streptococcus pneumoniae is present is pneumonia, a lung disease. Symptoms that occur when you get pneumonia are chills, and fevers, coughing, short or rapid breathing, pains in the chest, or even some of the same symptoms as the flu, like nausea, vomiting, headaches, and being overly tired. People that are most likely to get pneumonia are kids under two years old, or adults over 65. When having other medical conditions it is easier to get pneumonia when caused by Streptococcus pneumoniae. Bacteremia is a complication that can occur with the bacteria in the lungs, when it invades the bloodstream. It will for sure cause heart problems, and maybe even some other lung problems. [10]
Bacterial meningitis is also a commonly known disease, Streptococcus pneumoniae being one of the top causes for it. It is a very harmful infection in the fluid of the spinal cord, and can affect the fluid surrounding a person’s brain. It can be gotten from contact with discharges from someone’s nose or throat who has bacterial meningitis. Luckily, it is not terribly contagious, it requires pretty direct contact to catch. People with it are discovered by using spinal taps. Symptoms are some of the same as pneumonia, like high fever and a headache, one different one is a stiff neck. Also, similarly, nausea, vomit, light sensitivity, tiredness, and confusion are some of the other symptoms of bacterial meningitis. It is really common for babies to be able to get it, and some of the symptoms are different in babies. It is most common in babies and kids, but anyone can get it; and anyone who gets it can get seizures. [11]
Gallery
References
- Streptococcus pneumoniae by NationMaster. NationMaster.com 2003-5. 2/21/09
- Streptococcus pneumoniae by Kenneth Todar. Todar's Online Textbook of Bacteriology. 2008. 2/22/09.
- Gram Positive by Answers.com. http://www.answers.com. 2009. 2/22/09.
- Discovery of key proteins shape by Bio-Medicine. http://www.bio-medicine.org. © 2003-2009. 2/22/09.
- Herd Immunity by S.E. Smith. Conjecture corporation. © 2003 - 2009. 2/22/09.
- Streptococcus pneumoniae by Antigenics inc. http://qs21.com. © 2008. 2/21/09.
- Microbiology and pathogenesis of Streptococcus pneumoniae by Elaine I Tuomanen. Up2date. January 27, 2007. 2/27/09.
- Shuttle brings space-grown strep bacteria back for study by Jim Kelly. EurekAlert. Aug. 22, 2007. 2/27/09.
- Pneumococcal Pneumonia by doctors at MedicineNet.com. http://www.medicinenet.com. 8/14/08. 3/30/09.
- Bacterial Meningitis Directors of Health Promotion and Education. http://www.dhpe.org/. 3/30/09.



